Understanding Biofilm and Bacterial Contamination
The Hidden Threat in Your Dental Unit Waterlines
Every day, dental professionals rely on water flowing through their unit waterlines to provide safe, clean irrigation during procedures. However, lurking within these seemingly clean water systems is a microscopic threat that many dental practices overlook: biofilm. This invisible menace can harbor dangerous bacteria and compromise patient safety, making it essential for every dental office to understand what biofilm is, why it forms, and how to combat it effectively.
What Exactly Is Biofilm?
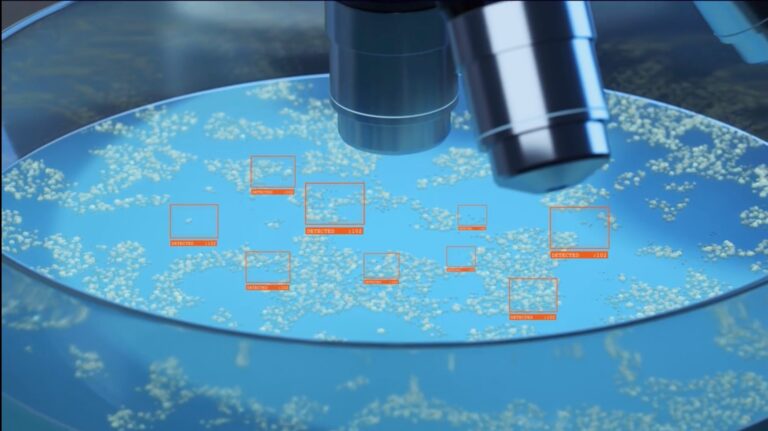
Imagine a bustling microscopic city where bacteria have built their own protective fortress. That’s essentially what biofilm represents. Biofilm is a thin, slimy layer composed of microorganisms that adhere to surfaces and embed themselves within a self-produced matrix of protective substances. This matrix, made up of proteins, polysaccharides, and DNA, acts like a shield that protects the bacteria from external threats, including disinfectants and antibiotics.
Unlike free-floating bacteria that drift individually through water, biofilm bacteria are organized communities that communicate with each other through a process called quorum sensing. They share nutrients, exchange genetic material, and work together to ensure their survival. This collaborative behavior makes biofilm bacteria significantly more resilient and dangerous than their planktonic (free-floating) counterparts.
In dental unit waterlines, biofilm forms as a sticky, often invisible coating on the interior surfaces of tubing, reservoirs, and other water system components. While you might not see it with the naked eye, this biofilm can be teeming with potentially harmful microorganisms that pose serious risks to both patients and dental staff.
The Perfect Storm: Why Dental Waterlines Are Biofilm Magnets
Dental unit waterlines create an almost ideal environment for biofilm formation. Several factors contribute to this perfect storm of conditions that bacteria love.
First, the narrow diameter of dental waterlines creates a high surface-area-to-volume ratio. This means there’s plenty of surface space for bacteria to attach and colonize relative to the amount of water flowing through the system. The more surface area available, the more real estate bacteria have to establish their communities.
Second, dental waterlines often experience periods of stagnation, particularly overnight, during weekends, or between patients. During these quiet periods, water sits motionless in the lines, giving bacteria ample time to attach to surfaces and begin forming biofilm. Even brief periods of low flow can provide enough opportunity for initial bacterial attachment to occur.
The temperature in most dental offices provides another advantage to bacteria. Room temperature water systems typically maintain temperatures between 68-72°F, which falls within the optimal growth range for many microorganisms commonly found in biofilm.
Additionally, dental waterlines can introduce nutrients that bacteria need to thrive. These nutrients might come from various sources, including the municipal water supply, backflow from patient oral cavities, or even the materials used in the waterline system itself.
Finally, the complex network of tubing, connectors, and reservoirs in dental units creates numerous surfaces and crevices where bacteria can hide and multiply. These areas can be difficult to clean thoroughly, providing safe havens for biofilm development.
What Bacteria are Lurking in Your Lines?
Biofilm in dental waterlines doesn’t just harbor harmless bacteria. Numerous potentially pathogenic microorganisms that can thrive within these protective communities, creating significant health risks for patients and staff.
Legionella pneumophila stands as one of the most concerning inhabitants of dental waterline biofilm. This bacterium causes Legionnaires’ disease, a severe form of pneumonia that can be fatal, particularly in immunocompromised patients or elderly individuals. Legionella thrives in warm water environments and can become aerosolized during dental procedures, making it especially dangerous in dental settings.
Pseudomonas aeruginosa represents another serious threat commonly found in dental waterline biofilm. This opportunistic pathogen can cause infections in wounds, the respiratory tract, and other body systems. It’s particularly dangerous for patients with compromised immune systems, chronic diseases, or open wounds in their mouths.
Mycobacterium species, including some that cause tuberculosis-like infections, have also been isolated from dental waterline biofilm. These slow-growing bacteria can cause chronic infections that are difficult to diagnose and treat.
Non-tuberculous mycobacteria (NTM) deserve special attention because they’re increasingly recognized as emerging pathogens in healthcare settings. These organisms can cause pulmonary infections that mimic tuberculosis but are often more resistant to standard treatments.
Other concerning microorganisms that may inhabit dental waterline biofilm include various species of Acinetobacter, Stenotrophomonas, and even some fungi and viruses. The diversity of potential pathogens underscores the importance of maintaining clean waterlines.
What makes these biofilm-associated bacteria particularly dangerous is their increased resistance to standard disinfection methods. The protective matrix surrounding biofilm bacteria can reduce the effectiveness of chemical disinfectants by up to 1,000 times compared to the same disinfectants used against free-floating bacteria.
The Health Risks: More Than Just a Theoretical Concern
The presence of pathogenic bacteria in dental waterline biofilm isn’t merely an academic concern—it represents a real and documented threat to patient and staff health. Multiple cases of infections linked to contaminated dental water have been reported in medical literature, highlighting the serious nature of this issue.
- CDC Official Documentation – CDC Best Practices for Dental Unit Water Quality (November 2024): CDC confirms that contaminated dental water has been linked to Mycobacteria outbreaks in children and case reports document infections with Mycobacteria and Legionella following various dental procedures.
- California Outbreak (2016) – PMC Study: “Invasive Mycobacterium abscessus Outbreak at a Pediatric Dental Clinic”: The largest documented outbreak of Mycobacterium abscessus odontogenic infections from a single pediatric dental clinic, affecting 71 patients (22 confirmed, 49 probable) with a median age of 6 years.
- Georgia Outbreak (2015) – CDC MMWR Report: CDC documentation of Mycobacterium abscessus infections among 24 children aged 4-8 years at a single pediatric dentistry practice in Georgia.
- Clinical Outcomes Study – PMC: “Outbreak of Invasive Nontuberculous Mycobacterium Infections”: Documents severe outcomes from the California outbreak where 70 of 71 patients required hospitalization and surgical debridement, with permanent tooth loss in 45 of 65 cases (1-6 teeth lost per patient).
- Additional Case Reports – PMC: “Healthcare-associated viral and bacterial infections in dentistry”: Reports on Pseudomonas aeruginosa infections including two cancer patients who developed gingival abscesses and 78 healthy patients who were colonized for 3-5 weeks after treatment with contaminated dental water.
Patients with compromised immune systems face the highest risk. This includes elderly patients, those undergoing cancer treatment, individuals with HIV/AIDS, patients with diabetes, and anyone taking immunosuppressive medications. For these vulnerable populations, exposure to contaminated dental water can lead to serious infections that might not affect healthy individuals.
Respiratory infections represent the most common type of illness associated with contaminated dental water. When contaminated water is aerosolized during procedures using air-water syringes, ultrasonic scalers, or high-speed hand pieces, patients and staff can inhale these contaminated droplets. This can lead to pneumonia, particularly in susceptible individuals.
Wound infections can occur when contaminated water comes into contact with open areas in the mouth, such as extraction sites, periodontal pockets, or areas where oral surgery has been performed. These infections can delay healing, cause significant pain, and may require additional treatment with antibiotics.
Healthcare workers are also at risk. Dental professionals who are regularly exposed to aerosols from contaminated waterlines may develop respiratory infections or other health problems. This occupational exposure represents a significant workplace safety concern that practices must address.
Current Standards and Guidelines: What You Need to Know
Recognizing the serious nature of waterline contamination, several organizations have established guidelines and standards for dental water quality. Understanding these requirements is crucial for maintaining compliance and ensuring patient safety.
The Centers for Disease Control and Prevention (CDC) recommends that dental units deliver water meeting EPA standards for drinking water. Specifically, this means water should contain no more than 500 colony-forming units (CFU) of aerobic mesophilic heterotrophic bacteria per milliliter. This standard applies to water used for non-surgical dental procedures.
For surgical procedures, the CDC recommends using sterile water or sterile saline as a coolant and irrigant. This higher standard reflects the increased risk associated with surgical procedures where contaminated water might enter open tissues.
The American Dental Association (ADA) has endorsed similar guidelines and emphasizes the importance of following manufacturer recommendations for waterline maintenance. The ADA also supports regular monitoring of water quality to ensure compliance with established standards.
The Occupational Safety and Health Administration (OSHA) addresses waterline contamination as part of its bloodborne pathogen standard, recognizing that contaminated water represents a potential occupational health hazard for dental workers.
Many state dental boards have incorporated these federal guidelines into their regulations, making compliance a legal requirement rather than just a best practice recommendation.
Georgia is the most recent state to pass legislation requiring regular water line testing, record keeping, and verification by an independent lab. Other states are moving closer and closer to enacting baseline regulations for water safety in dental offices.
Testing Methodologies: How to Monitor Your Water Quality
Regular testing represents the only reliable way to determine whether your dental waterlines are harboring dangerous levels of bacteria. Several testing methods are available, each with its own advantages and considerations.
Some practices use in-office testing kits (such as paddles) that can provide preliminary results within hours. While these rapid tests are convenient, they aren’t as comprehensive or accurate as laboratory-based testing methods. The results and records may not provide an adequate defense in the case of litigation. And, these tests require significant training, time, and detailed work from dental professionals.
DentiSafe uses the R2A test method and we’re the only EPA-certified independent lab serving the dental industry today. R2A is the gold-standard for water testing in part because it catches the slow-growing bacteria that quick tests won’t. The biggest disadvantage of R2A testing is that it takes 120 hours to complete the testing protocol. That’s why we developed FASTRead, an early notification (in the first 24 hours of testing) if your water sample shows clear signs of bacterial contamination that will exceed the acceptable limits.
Read more on our FAQ page about the most readily available and reliable testing methods available today.
When collecting samples for testing, proper technique is crucial to ensure accurate results. Samples should be collected using sterile containers and techniques to avoid contamination. The timing of sample collection is also important—samples collected after periods of stagnation may show higher bacterial counts than those collected during active use.
Taking Action: Protecting Your Practice and Patients
Understanding biofilm and its dangers is only the first step. Soon, every dental practice will need to implement comprehensive strategies to prevent biofilm formation and maintain water quality that meets safety standards.
Regular waterline maintenance represents the foundation of any effective contamination control program. This includes following manufacturer recommendations for cleaning and disinfection, replacing waterline components according to established schedules, and ensuring proper training for all staff members involved in waterline maintenance.
Chemical treatment systems can help prevent biofilm formation and eliminate existing contamination. Various products are available, including continuous-flow disinfectants, shock treatments, and specialized cleaning solutions designed specifically for dental waterlines.
Regular monitoring through appropriate testing methods ensures that contamination control measures are working effectively. Practices should establish testing protocols, maintain detailed records, and be prepared to take corrective action if test results indicate problems. DentiSafe provides a streamlined solution that makes all of this as easy as possible for busy dental professionals. You get the gold-standard testing, safe and secure record keeping, access to experts if there’s an issue, and a total package that’s very affordable.
In any case, staff education is crucial for success. All team members should understand the importance of waterline maintenance and their role in preventing contamination. Regular training updates help ensure that everyone stays current with best practices and regulatory requirements. The DentiSafe team is working hard to be an education-first company. Our mission translates into safer water for everyone: patients and dental professionals.
The invisible threat of biofilm in dental waterlines represents a serious challenge that every dental practice must address. By understanding what biofilm is, recognizing the risks it poses, and implementing appropriate prevention and monitoring strategies, dental professionals can protect their patients, staff, and practices from this hidden danger. The investment in proper waterline management is not just about regulatory compliance—it’s about maintaining the highest standards of patient care and safety that define excellent dental practice.
DentiSafe has a streamlined, comprehensive, reliable solution for your office
Explore our convenient subscription service for water testing or shop for individual kits. As the only EPA-certified independent lab serving the dental industry we offer the gold-standard testing method, highly responsive service, and everything you need to make water testing painless and reliable.